
Photo courtesy: World Health Organisation
By the time of writing, less than 3 percent of Africa’s 1.3 billion inhabitants have been fully vaccinated against COVID-19, in contrast to a world average of 30 percent fully vaccinated. Rapidly scaling up COVID-19 vaccine programmes in Africa will require sustained collaboration between health and finance officials as they plan, budget and implement these programmes.
In March 2021, we pointed out that most governments in Africa had not yet budgeted for COVID-19 vaccines. In April 2021, we cautioned that not budgeting timeously and relying on rushed reprioritisation of funds may crowd out priority expenditure, including other health and vaccine programmes. And, at the same time, noted that allocating domestic resources will be necessary to address the vaccine financing gap and will be an important signal of commitment to the international development community and catalyse greater external support.
There are many reasons why COVID-19 vaccine programmes may not have been budgeted for or included in budget documents. Some governments assumed that international support, particularly through COVAX, would have been sufficient. Others, albeit unofficially, expressed that their already limited fiscal envelope needed to be allocated to other pressing priorities, particularly given that official numbers of confirmed cases in their countries remained relatively low. There is also likely to be spending related to the vaccination programmes that is happening off-budget; development-partner funding in particular may not reflect in budget documents if partners have opted not to channel their funds through country systems and if countries have reprogrammed existing loans or grants to their vaccination programmes.
However, our latest round of data collected for the COVID-19 Africa Public Finance Response Monitor paints a more promising picture of African governments’ including COVID-19 vaccination programmes in their budget documents. The Monitor captures information for 18 African countries that have publicly included the vaccine programmes through either annual or supplementary budgets. There is also indication that countries are allocating more of their own resources. By July 2021, Algeria had budgeted USD 174.6 million (0.1 % of GDP) for its COVID-19 vaccine programme. In February 2021, The Ministry of Finance in Cabo Verde stated that it had budgeted USD 2.2 million (0.11% of GDP) for the acquisition of COVID-19 vaccines. Ghana’s 2021 budget presented to Parliament in March 2021 had an amount of USD 165 million to cover both operational and procurement costs. In June 2021, three months after passing the annual budget, Nigerian lawmakers approved a supplementary budget including USD 111 million for the COVID-19 vaccine programme. This will be financed through existing grants and loans and special reserve accounts. In Uganda’s 2020/21 budget around USD 139 million (0.4% of GDP) was allocated to vaccine procurement and in FY21/22 around USD 132 million (0.3% of GDP). It is unclear how much of the 2020/21 budget was expensed or rolled over.
As seen in figures 1 and 2, it is apparent that the amounts vary significantly even when accounting for GDP and population size.
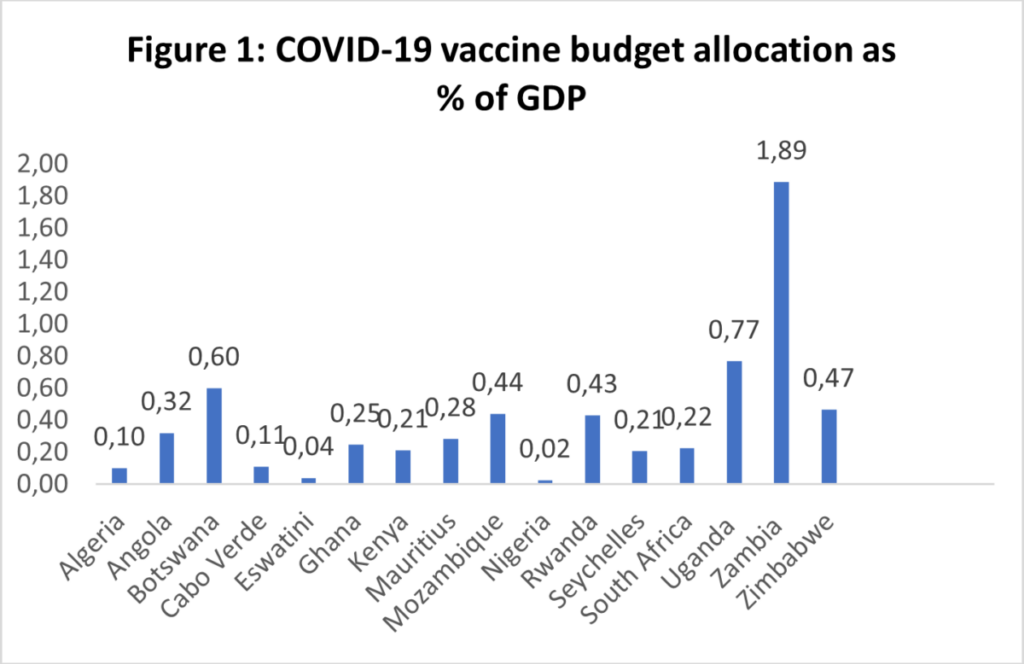
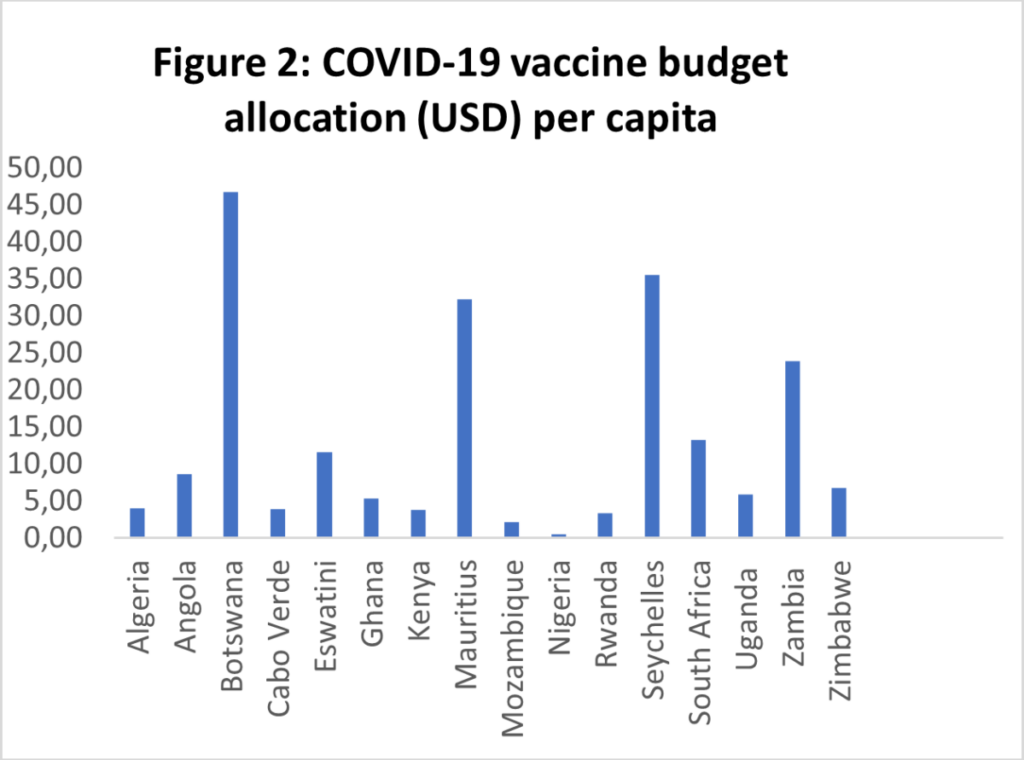
Sources: COVID-19 Africa Public Finance Response Monitor; Statista
In a handful of countries, we are also starting to see funds being allocated to creating vaccine manufacturing capacity. In Ghana’s mid-term budget review statement, it was announced that USD 25 million in seed funding has been committed to establishing a National Vaccine Institute; however, the impact may be limited when it comes to the short or even medium-term provision of COVID-19 vaccines. The Moroccan government allocated USD 500 million to encourage domestic manufacturing of the COVID-19 vaccine. Senegal will build a vaccine manufacturing hub, with the ability to produce COVID-19 vaccines; the cost of this is estimated at EUR200 million and is primarily funded by development partners. The Mauritian government has also allocated USD 28 million to encourage domestic manufacturing of the COVID-19 vaccine and other pharmaceutical products. These investments in manufacturing are a promising indication that this crisis is being used to create resilient and self-reliant health systems in Africa. However, to ensure these facilities do not end up as “white elephants”, governments will need to ensure adequate local ownership and investment and maintain predictable and sustainable partnerships with the international development community and private sector.
That said, and given the mammoth task of reaching population immunity in Africa, significantly more funding will need to be channelled to the immediate tasks of procuring vaccines and distributing them. While by the middle of 2021, supply constraints remained the dominant hindrance to vaccinating Africa’s population, we’re increasingly seeing instances of countries unable to administer the supplies allocated to them.
While the reasons for this extend beyond the purview of PFM or even the minister of finance, we do know that more resources for operational costs and combatting vaccine hesitancy need to be mobilised and potentially reallocated from existing non-essential budget items. Getting shots into arms is expensive business: the WHO has estimated that 60 cents of each dollar for delivering vaccines is needed for operations. They also observed that while most African governments have financing plans to cover the initial three percent of their populations, these plans do not adequately cover subsequent phases of the roll out. The WHO also cautions that the costing plans they’ve reviewed typically exclude key cost drivers of getting shots into the arms of people in peripheral areas, such as recruiting vaccinators, cold-chain storage, and transport. This is of fairly grave concern, as development-partner funding for operational costs or last-mile distribution of vaccines isn’t typically abundant, and that appears to be the case with the COVID-19 vaccine too. It also implies that vaccine inequity within countries is set to deepen as those outside of urban areas may not have access to the vaccines or be sensitised to the need to be vaccinated.
There are also those who, in recognising the extent and expense of vaccinating 60 percent of Africa’s population (or 84 percent for those who argue that is the minimum threshold against the Delta variant), doubt population immunity will be reached in Africa in the medium term. The World Bank has estimated that average vaccination costs per capita across Africa is approximately 150% of the annual total government health expenditure per capita of African governments. While this figure represents the significant burden of vaccinating against COVID-19, it is also a reminder of the inadequate funding currently being channelled to health in Africa. While we slowly progress to some semblance of population immunity, we need to ensure that additional financing is allocated to health systems to ensure adequate treatment for those who, due to not receiving protection from a vaccine, fall severely ill with COVID-19.
A forthcoming CABRI paper, Budgeting in the context of COVID-19: Trends and tools of reallocations, will show, increases in budget allocations to the health sector for the COVID-19 response have been a common practice throughout the crisis. Large investments were announced for prevention and treatment needs, such as personal protective equipment, testing kits, ventilators, and isolation or quarantine facilities. Health spending as a share of budget allocation reached 12.1 percent in Mozambique, against an average 8.9 percent in the last decade. Even Seychelles, which already had the highest level of expenditure on health per capita on the continent, at USD 792 per head in the pre-COVID context, increased the share of recurrent expenditure allocated to health from 16.8 percent to 17.3 percent, while it decreased for most other budget items. Ethiopia raised its health budget by 46 percent in 2020. Kenya reallocated USD 9.4 million towards employment of new health workers. A significant share was also allocated to health staff, either for salary supplements or hiring of extra staff, in Kenya, Malawi, South Africa and Zambia. Egypt increased its health spending in 2021/22 to almost USD 7 billion, up from 5.9 billion in 2020/2021.
However, the reprioritisation to the health response did not usually translate into an increase for other non-COVID-related health programmes. Instead, the focus on the COVID-19 response sometimes translated into a neglect of other diseases. What is required is an overall increase to the health sector as both a complement to and prerequisite for vaccination as a means to save lives. Reprioritisation also, at times, came at the expense of social and human capital sectors, such as education and nutrition.
On 30 September, we will as we did in April 2021, convene ministries of finance and health across Africa to reflect on the aforementioned challenges and share where they find themselves now in terms of COVID-19 vaccine financing, procurement and distribution.